Rheumatoid Vasculitis (RV)
Updated and reviewed by
Dr Richard Watts
Consultant Rheumatologist – Ipswich Hospital
Last updated June 2016
What is Rheumatoid Vasculitis?
Rheumatoid Vasculitis (RV) is a serious complication of rheumatoid arthritis (RA) where there is inflammation of the blood vessels. It commonly affects the skin causing rash and ulcers and the nerves causing loss of sensation although any part of the body may be involved.
Who are affected?
RV is reported to be commoner in men with rheumatoid arthritis (1 in 9 men in one study) than in women (1 in 38 women in one study) but appears to be becoming much rarer over the last few decades with better treatment of RA. Patients with rheumatoid factor antibodies, rheumatoid nodules and long standing RA are most likely to develop RV. Patients who develop Felty’s Syndrome (a combination of rheumatoid arthritis, large spleen and low neutrophil count in the blood) are also more likely to develop RV. There is also an association with smoking.
What are the symptoms?
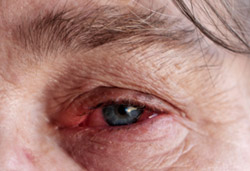
The symptoms will depend upon the part of the body affected. Skin rashes and ulcers are a common problem. Involvement of the nerves usually causes numbness or tingling and “pins and needles” symptoms, muscle weakness may also develop. Inflammation may develop around the outside of the heart (pericarditis) which can cause chest pain. Inflammation in the eyes may cause pain, redness and impaired vision. Rarely the kidneys may be involved causing blood and protein in the urine or kidney failure.
Non-specific features may include fatigue, fevers and weight loss.
What is the aetiology (cause)?
The cause of RV is not yet known. In RV it has been noted that there are more likely to be particular types of antibodies in the blood and they will be at a higher level than in rheumatoid arthritis patients without RV. A link with smoking has been noted and some researchers suggest that smoking leads to damage to the lining of the blood vessels that pre-disposes to developing RV.
Making a diagnosis
There is no specific test for diagnosing RV. Blood tests may show evidence of inflammation and high levels of some antibodies but these are not specific for RV. A biopsy of an affected tissue or organ (skin, muscle, nerve, kidney etc) may confirm vasculitis but again may not be specific for RV and other types of vasculitis should be excluded. Neurophysiology tests (electrical tests of nerves and muscles) may show evidence of inflammation and sometimes be used to guide a biopsy. Angiography (x-ray or other imaging of the blood vessels) may show non-specific evidence of vasculitis.
Treatment
Treatment depends on the severity of the vasculitis and the organs involved. Mild RV affecting only skin or peripheral nerves may be treated with steroids and immunosuppressants such as methotrexate or azathioprine. Severe RV may need treatment with high dose steroids and cyclophosphamide. Newer drugs such as anti-TNF antibodies and rituximab have also been successfully used in RV in combination with other drugs.
Stopping smoking is essential.
Drugs and Side effects
For information on the main drugs prescribed for Rheumatoid Vasculitis see:
For information on other drugs used in the treatment of vasculitis see Glossary of drugs and side effects.
Prognosis
The prognosis in RV depends in part on the severity of the damage to the organs involved. RV may also increase the risk of developing cardiovascular disease. Some previous studies have suggested that the development of RV in a patient with rheumatoid arthritis may have a significantly worse prognosis than rheumatoid arthritis patients without RV.
Key points
- RV is part of rheumatoid arthritis in some patients
- Treatment and prognosis depend on the disease severity
- Stopping smoking is critical
Acknowledgements
Vasculitis UK for providing the information.
