Polymyalgia Rheumatica (PMR)
What is Polymyalgia Rheumatica?
Polymyalgia Rheumatica (PMR) is an inflammatory disorder. It is frequently linked to Giant Cell Arteritis (GCA) occurring in 50 per cent of patients with GCA. Approximately 15 per cent of PMR patients develop GCA.
Who are affected?
The disease is usually diagnosed in patients over the age of 65. It is rarely seen in patients younger than 50. Women are twice as likely to develop PMR as men.
What is the aetiology (cause)?
The cause of PMR is not yet known.
What are the symptoms?
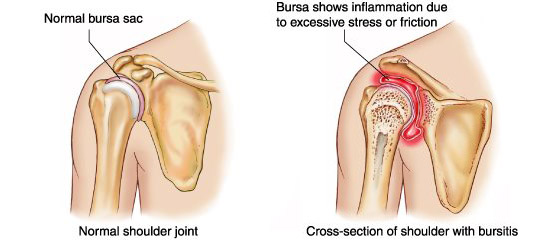
The symptoms usually come on over a few days. Symptoms include aching muscles and morning stiffness in the shoulders, hips, neck and mid-body. Other symptoms reported include: general tiredness, weakness, weight loss, low grade fever. Inflammation of the bones and joints can cause difficulty moving. Some patients develop swelling or fluid retention (oedema) of the hands, wrists, ankles and top of the feet.
Making a diagnosis
There are no specific tests for PMR. Blood tests may show evidence of inflammation. Ultrasound and Positron emission tomography (PET scanning) have been used to confirm PMR inflammation. Patients with only PMR do not have the symptoms of GCA therefore a biopsy of the temporal artery (necessary in GCA) is unnecessary in PMR.
Treatment
Moderate to high doses of steroid drugs (prednisolone) improve the symptoms of PMR. The effective dose is maintained for several weeks after the symptoms have resolved. Then it is gradually lowered and stopped. Careful monitoring is required in case the symptoms recur.
Where long term use of steroids or side effects occur the use of Methotrexate may allow the dose of steroid to be reduced. Ibuprofen (an anti-inflammatory drug) can be used to reduce painful symptoms, especially when the symptoms are only mild.
Drugs and Side effects
For information on the main drugs prescribed for Polymyalgia Rheumatica see:
For information on other drugs used in the treatment of vasculitis see Glossary of drugs and side effects.
Prognosis
Relapse occurs in 25 to 50 per cent of patients. This is more likely if the steroid dose is reduced too quickly. Relapse requires restarting or increasing the steroid dose. In most cases the symptoms will cease within one month to one year. The steroids can then be discontinued.
Key Points
- PMR is sometimes associated with Giant Cell Arteritis
- Treatment is usually with steroids
- Treatment may be able to be stopped once the disease is controlled.
Related Vasculitis Articles
- Fertility and Vasculitis – Dr David Jayne
Further reading
- Treatment of Polymyalgia Rheumatica: A Systematic Review – José Hernández-Rodríguez, MD, PhD; Maria C. Cid, MD, PhD; Alfons López-Soto, MD, et al
- Clinical, radiological, and biochemical characteristics in patients with diseases mimicking polymyalgia rheumatica – Hidekatsu Yanai, Hiroshi Yoshida, and Norio Tada
- Large Vessel Diseases – Shima Gulati, Arvind Bagga
Useful links
Our Useful Vasculitis Links page contains contact details for organisations offering help and support for patients with Polymyalgia Rheumatica, Giant Cell Arteritis and other vasculitis diseases.
Acknowledgements
Vasculitis UK for providing the information.
